- Home
- Research
- Find research
- Edina Sehic: The future of an artificial uterus
Edina Sehic: The future of an artificial uterus
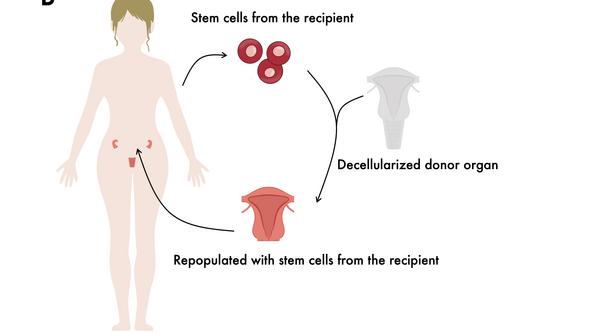
Transplants rely on donors while recipients face lifelong immunosuppressive treatment. Edina Sehic is exploring an alternative that addresses both issues: crafting an artificial uterus from a patient’s own cells.

EDINA SEHIC
Dissertation defense: 19 January 2024 (click for more info)
Doctoral thesis: Uterine tissue engineering: Translational approaches using animal models
Research area: Obstetrics and Gynecology
Sahlgrenska Academy, The Institute of Clinical Sciences
What is the backstory behind your research?
“Many women struggle with infertility due to uterine dysfunction, arising from post-surgical damage, congenital absence, or cancer-related removal. These conditions often lead to infertility treatable solely through uterus transplantation. However, this procedure carries significant risks and side effects,” says Edina Sehic.
Utilizing the patient’s cells
Under Professor Mats Brännström’s guidance, Gothenburg became the pioneer in uterus transplants in 2012. Edina Sehic, a pharmacist and molecular biologist, is currently a PhD student in Brännström’s group at the Sahlgrenska University Hospital.
“Our research aims to create a patient-specific artificial uterus made from the individual’s own cells. This approach sidesteps the risks tied to immunosuppressive treatment and eliminates the need for a donor. We are also exploring an option where patient-specific uterine biomaterial could replace a damaged segment rather than requiring a complete uterus transplant.”
Assessed on larger animal models
Could you summarize the primary focus of your PhD project?
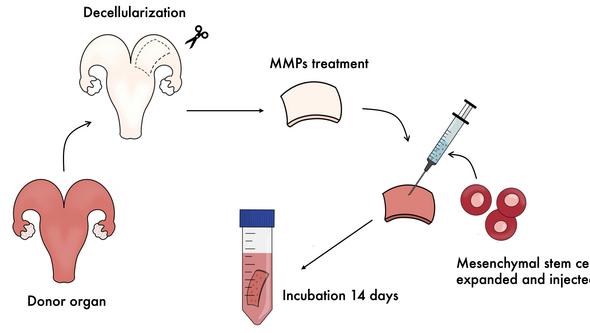
“My thesis centers on creating biomaterials for repairing a damaged uterus, by scaling our previous findings into larger animal models. The uterine material, previously assessed and transplanted into rats, has now undergone evaluation in sheep,” explains Edina Sehic.
“I have also further developed protocols for producing our material using tissue from cows and baboons, to ensure the protocols’ readiness for human applications soon. Evaluating materials across various animal species helps assess production safety and efficacy.”
“Constructing a complete uterus”
What are the key outcomes of your research?
“We have successfully translated our prior studies from rat models to larger animal models. This is crucial for effectively producing biomaterials for future clinical applications. Additionally, our research has deepened our understanding of the immune system’s response to our material and its implications.”
What patient benefit will this research result in?
“In the future, our research will not only assist women with damaged uteruses in achieving pregnancy. Our findings also provide insights into the body’s regenerative processes, and how we can design tools and materials to create patient-adapted grafts,” says Edina Sehic, adding:
“Once we achieve our interim goal of producing a section of the uterus and accumulate sufficient knowledge, the next step is to construct a complete uterus. Such advancement could replace the need for a donor in a uterus transplant, minimizing risks for patients and reducing dependency on organ availability.”
Text: Jakob Lundberg