Link directly to the thesis in GUPEA
ABSTRACT
Intraepidermal carcinoma (IEC), also known as Bowen disease (BD) or squamous cell carcinoma (SCC) in situ, is a precursor to SCC. The incidence of IEC is increasing rapidly in fair-skinned populations with a subsequent increase in patient morbidity. This calls for optimized patient management through improving diagnosis and choosing the most advantageous treatment. A key step is making a correct diagnosis, which is best accomplished using dermoscopy prior to histopathological confirmation. Several treatment options are available for IEC, e.g. photodynamic therapy (PDT), surgical excision and destructive methods like cryosurgery and curettage. The purpose of this thesis was to evaluate the agreement between dermatologists on the dermoscopic findings of IEC as well as the effectiveness of PDT, surgical excisions and a comparison between cryosurgery and curettage.
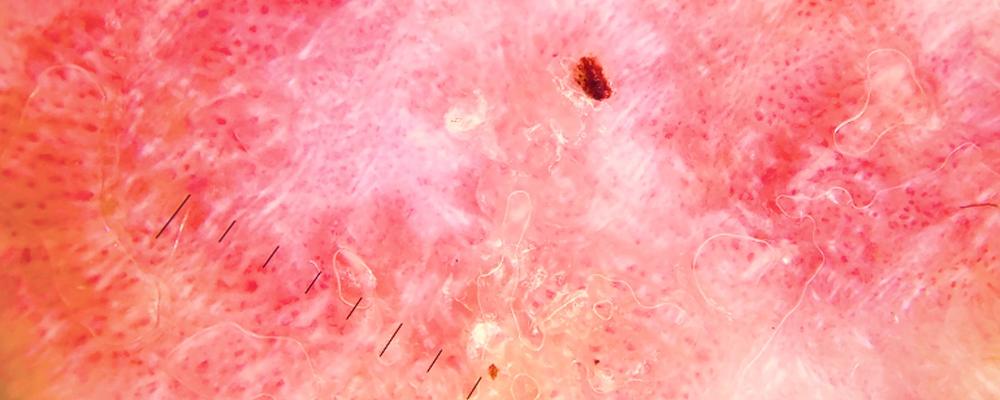
In Paper I, we measured the interobserver agreement between international dermatologists on dermoscopic findings in IEC. The frequency of pre-defined dermoscopic findings were: scales (83%), dotted/glomerular vessels (77%), pinkish-white areas (73%), and hemorrhage (46%). The interobserver agreement ranged from poor to moderate with the highest Kappa values noted for scales (0.55) and hemorrhage (0.54), while pinkish-white areas showed the lowest Kappa value (0.015).
In Paper II, we assessed the effectiveness, recurrence risk, and factors affecting the response rate of PDT for IEC. PDT is a relatively effective treatment modality with an overall clearance rate of 63.4%. Larger lesions (>20 mm) and a single PDT session were risk factors for unsuccessful treatment. In
Paper III, we aimed to evaluate the clinicopathological risk factors for incomplete excision of IEC. Less surgical experience was independently associated with incomplete surgical excisions using a less strict definition (mild to moderate dysplasia at the resection margin), whereas less experience and location on the head and neck area or upper extremities was independently associated with incomplete excision using a strict definition (no dysplasia at the resection margin).
In Paper IV, we performed a randomized controlled trial to compare the effectiveness of cryosurgery and curettage for IEC. The overall clearance rate 1 year after cryosurgery was significantly higher than with curettage (94.6% vs 78.9%). Nevertheless, wound healing times were significantly shorter with curettage.
In conclusion, the interobserver agreement for dermoscopic findings of IEC is poor to moderate. PDT provides clearance in approximately two-thirds of the treated IECs. Risk factors for incomplete excisions of IEC are less experienced surgeons and location on the head and neck area or upper extremities. Cryosurgery and curettage both show high clearance rates, with cryosurgery being significantly more effective and wound healing times being shorter with curettage.