Endometrial Cancer - Studies on recurrences, complications and preoperative diagnostics
On Mars 31, Åsa Åkesson is defending her thesis for Doctor of Philosophy in Medical Science at the Institute of Clinical Sciences, Sahlgrenska Academy, in the research subject of Obstetrics and Gynecology
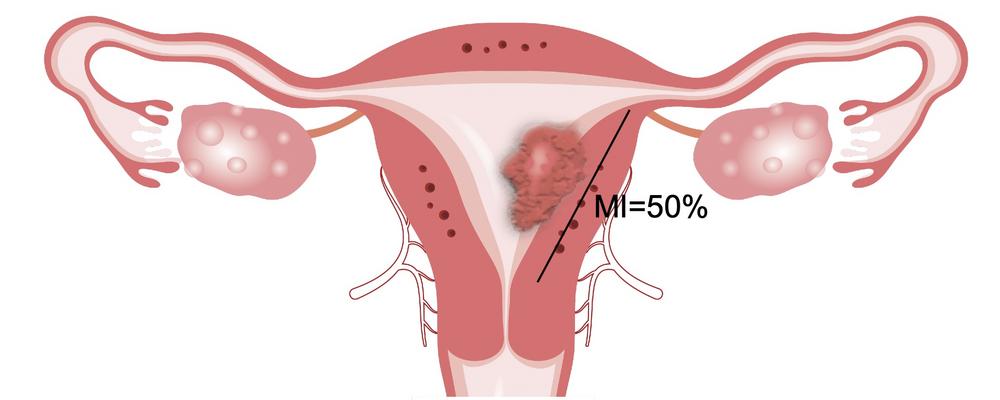
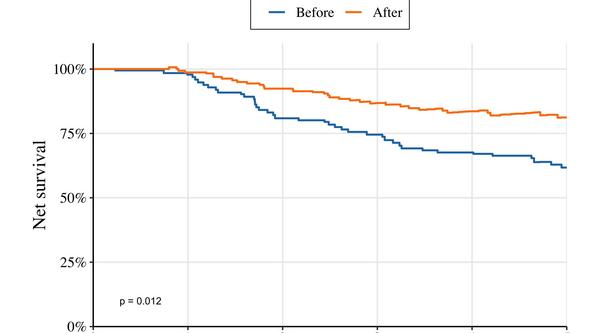
The title of the thesis is: Endometrial Cancer - Studies on recurrences, complications and preoperative diagnostics
MORE INFORMATION ABOUT THE DISSERTATION
Supervisor: Pernilla Dahm-Kähler
Co-Supervisors: Henrik Leonhardt and Ian Milsom
Opponent: Frédéric Amant, Katholieke Universiteit/University Leuven, Leuven, Belgium
Examining committee: Andreas Muth, Päivi Kannisto och Johan Stranne
Area
Health and
medicine