TAT - Radiation Physics
Short description
In preclinical studies, as well as in the clinical phase I study recently published, there are always different aspects of radiation physics that has to be regarded.
These aspects range from the radiation safety during handling of various radioactive sources, calculation of microdosimetric properties regarding irradiation of single cells, dosimetry and the determination of the absorbed dose to tumors, bone marrow or other normal tissues, estimate of the relative biological effectiveness (RBE) for various end-points, estimation of the maximum tolerated absorbed dose or activity for various treatment situations, and considerations regarding tumor cure probability for different treatments and therefore irradiation situations.
In the work in J Nucl Med 2006;47:1342–1350 calculations were done in order to estimate the absorbed dose to differently sized tumors.
Some examples of studies in which different aspects of radiation physics have been considered are presented below.
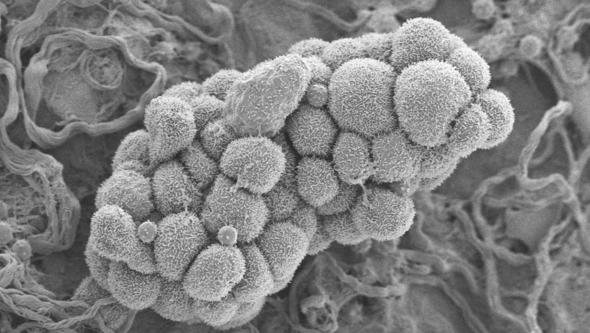
In the work in Med Phys 2004;31:218-225 a microdosimetric analysis of 211At irradiation of cancer cells was done. A custom-built computer program based on the Monte Carlo method was used to simulate the irradiation. The results show that 211Po atoms, created on a cell surface by the decay of 211At atoms, will diffuse from the cell during its life-span. The increasing distance to the cell nucleus will drastically decrease the probability of the emitted alpha particle to hit the cell nucleus. The conclusion was that for dispersed cells, the diffusion of 211Po atoms will reduce the total absorbed dose from cell-bound 211At by a factor of 2.
In the work in J Nucl Med 2005;46:464–471 the myelotoxicity and the RBE for alpha-particles emitted from 211At was investigated in a pre-clinical study. An RBE of 3.4 ± 0.6 and 5.0 ± 0.9 was found when comparison was made with electrons emitted from 99mTc or generated by gamma rays emitted from an external 60Co source. The end-point parameter was degree of myelosuppression.
Finally, in the work in J Nucl Med 2005;46:2061–2067 the aim was to evaluate the RBE of 211At compared with that of 60Co gamma-irradiation. The endpoint was growth inhibition (GI) of subcutaneous xenografts. The Balb/c received an intravenous injection of 211At-labeled monoclonal antibody MX35 F(ab')2 at different levels of radioactivity (0.33, 0.65, and 0.90 MBq). To calculate the mean absorbed dose to tumor, a separate biodistribution study established the uptake of 211At in tumors and organs at different times after injection. External irradiation of the tumors was performed with 60Co. The biodistribution study showed the uptake of the immunoconjugates by the tumor to be 14% after 7 h. At 40 h, the ratio of uptake in tumors to uptake in blood reached a maximum value of 6.2. The administered activities of 211At corresponded to absorbed doses in tumors of 1.35, 2.65, and 3.70 Gy. The value (mean ± SEM) for D37 was 1.59 ± 0.08 Gy. Tumor growth after 60Co external irradiation showed a value for D37 of 7.65 ± 1.0 Gy. The corresponding RBE of 211At irradiation was 4.8 ± 0.7.
Related Links
- American Association of Physicists in Medicine (External link)
- American Institute of Physics (External link)
- American Physical Society (External link)
- Conference of Radiation Control Program Directors (External link)
- Decay Radiation Search (External link)
- European Federation of Organizations for Medical Physics (External link)
- European Physical Society (External link)
- European Society for Radiotherapy & Oncology (ESTRO) (External link)
- European Spallation Source (External link)
- Geant4 (External link)
- Health Physics Society (External link)
- International Atomic Energy Agency (External link)
- International Commission on Non-Ionizing Radiation Protection (External link)
- International Commission on Radiation Units & Measurements (External link)
- International Radiation Protection Association (External link)
- Medical Physics Dictionary (External link)
- Nobel Prizes in Physics (External link)
- Nuclear Data Services (IAEA) (External link)
- Nuclear Decay Data in the MIRD Format (External link)
- Physics Today (External link)
- Physics World (External link)
- Radiation Effects Research Foundation (External link)
- Society of Nuclear Medicine (External link)
- Swedish Association of Medical Physicists (External link)
- Swedish Institute of Space Physics (External link)
- Swedish Physical Society (External link)
- Swedish Radiation Safety Authority (External link)
- The Physics Classroom (External link)
- United Nations Scientific Committee on the Effects of Atomic Radiation (External link)