
- Home
- Research
- Find research
- Hannah Ceder: Improving the management of high-risk basal carcinoma
Hannah Ceder: Improving the management of high-risk basal carcinoma
Less than ten percent of patients with high-risk basal cell carcinoma on the face receive the most effective treatment. Hannah Ceder’s research highlights how improved diagnostics and surgical methods can change that.

HANNAH CEDER
Dissertation defense: 11 June 2025 (click for details)
Doctoral thesis: Enhancing the management of high-risk basal carcinoma
Research area: Dermatology and Venereology
Sahlgrenska Academy, The Institute of Clinical Sciences
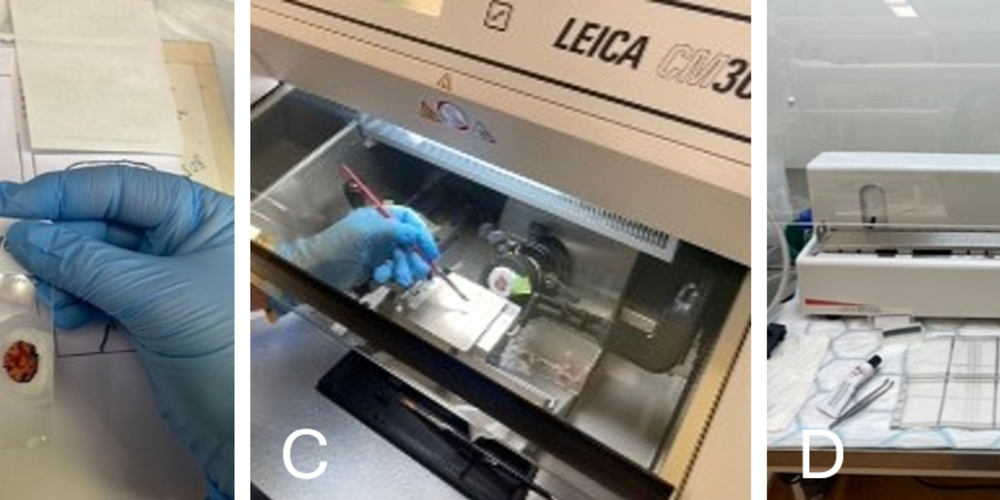
Basal cell carcinoma (BCC) is the most common form of cancer in Sweden and is increasing rapidly. The surgical method known as Mohs micrographic suregy (MMS)—where the tumor is removed layer by layer with microscopic control—is recommended for high-risk cases on the face. However, it is currently only offered in Gothenburg, Stockholm, and Lund, approximately 600 procedures per year in Sweden. This means that fewer than ten percent of the patients who should receive this treatment actuallydo.
“My research shows how we can identify the right patients for MMS early on, so they avoid undergoing repeated treatments with poorer outcomes,” says Hannah Ceder, dermatologist and Mohs surgeon at the Department of Dermatology at Sahlgrenska University Hospital and doctoral student at the Institute of Clinical Sciences.
Four studies on risks and diagnostics
Hannah Ceder’s thesis consists of four studies exploring:
- Risk factors for incomplete excisions.
- Differences between previously treated and untreated tumors.
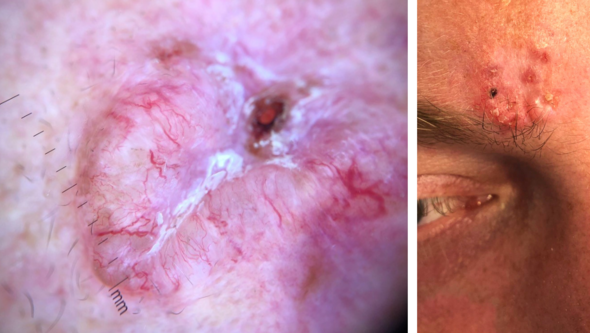
- How high-risk BCC can be identified through clinical and dermoscopic findings. Dermoscopic findings refer to skin changes observed using a dermoscope, a magnifying tool that provides a detailed view of the skin’s structure.
- Whether hyperspectral imaging, an advanced camera technique, can be used to better map the extent of tumors.

Tumor tissue left in one in five cases
One study analyzed 987 traditional surgeries for high-risk BCC. In 20.6 percent of the cases, tumor tissue was left behind after the procedure.
“It’s clear that we don’t always manage to remove the entire tumor with traditional surgery. Patients who have previously been treated also tend to end up with larger scars and require more Mohs stages than those operated on immediately. This highlights the importance of getting it right the first time.”
Algorithm improves diagnostic precision
In one of the studies, a diagnostic algorithm was developed to distinguish high-risk cases from other subtypes based on clinical and dermoscopic features The algorithm achieved a sensitivity of over 80 percent.
“This is an important step toward improving diagnostic accuracy. If we can identify the right patients before surgery, more of them can receive Mohs surgery and avoid ineffective treatments that don’t solve the problem,” says Hannah Ceder.
The fourth study showed that hyperspectral imaging, an advanced camera technique that analyzes different wavelengths of light, can help better map the tumor’s extent before surgery.
Imaging tools and clinical impact
What has been most rewarding during the doctoral project?
“One of the most rewarding parts has been trying to answer the questions that come up in my clinical work with basal cell carcinoma and MMS. Being able to make a difference for patients by ensuring they get the right treatment. Another important part has been using my research to spread knowledge about MMS, which ultimately benefits the patients.”
Text: Jakob Lundberg