- Home
- News and events
- Find news
- Person-centred communication improves consultations between health care professionals and patients. Article and researcher in focus: Monica Pettersson
Person-centred communication improves consultations between health care professionals and patients. Article and researcher in focus: Monica Pettersson
Person-centred communication improves consultations between health care professionals and patients. Article and researcher in focus: Monica Pettersson
 Article: Prepared for surgery - Communication in nurses’ pre-operative consultations with patients undergoing surgery for colorectal cancer after a person-centred intervention. Link to the article.
Article: Prepared for surgery - Communication in nurses’ pre-operative consultations with patients undergoing surgery for colorectal cancer after a person-centred intervention. Link to the article.
Researcher: Monica Pettersson
Appointment: Lecturer in combination with an appointment at the vascular surgery unit at the Sahlgrenska University Hospital. Monica became a docent recently and is a part-time researcher in vascular diseases.
Age: 55
Which personal resources do you use in your research? Since I am very interested in people, I am also very curious about them. It began with book that inspired me: Människan är en berättelse (The human is a narrative). Communication is very interesting; not least, body language and I enjoy discussing different topics. I actually wrote both my bachelor’s project and master’s thesis about body language between patients and physicians, and how it affects power structures and master suppression techniques.
Your research has been about person-centred communication and information to patients before undergoing surgery for colorectal cancer. Please tell me about this. For the past few years, I have been part of a project called Pincore, which is about person-centred information and communication to patients with colorectal cancer and how to support them to be better prepared for their surgery. This actual article is a process evaluation of the intervention and focuses on the consultations. For the analysis, we started by recording nurses’ and physicians’ consultations with patients. In addition, we collected survey data in order to measure quality of life, sense of context and preparedness pre-surgery. From these consultations, we could clearly see that patients were given very little space; at times, the communication was just one way.
We started the intervention by training all the staff during a couple of workshops at Sahlgrenska University hospital/Östra, Ersta hospital and Skaraborg hospital/Skövde. Person-centred care, the ethics and philosophy of personhood and person-centred communication were themes for these workshops. There was a particular focus on the structure of person-centred consultations. The introduction should always be the presentation of an agenda (created together with the patient) covering the content of the consultation. There should also be a clear ending to the consultation. By asking open-ended questions, the nurse then invites the patient into the consultation. Along with these workshops we developed a communication support tool for the consultations: a PEM (Patient education material) to be used at home by the patients in order to prepare them for the consultations. The PEM was developed during a PhD student project that involved patients in the design. We also recorded a film with a real patient who was very committed.
As a next step, we again recorded consultations and collected data in order to see if there was any difference. We observed that our PEM was used in about half of the 18 consultations. The structure of the consultations had improved significantly and did not unfold as they did before the intervention ”Now I am going to inform you about this, this and that.” However, the most difficult topics such as regarding the detection of the actual tumour was never discussed as recommended since it emerged that this was something the patients usually brought up.
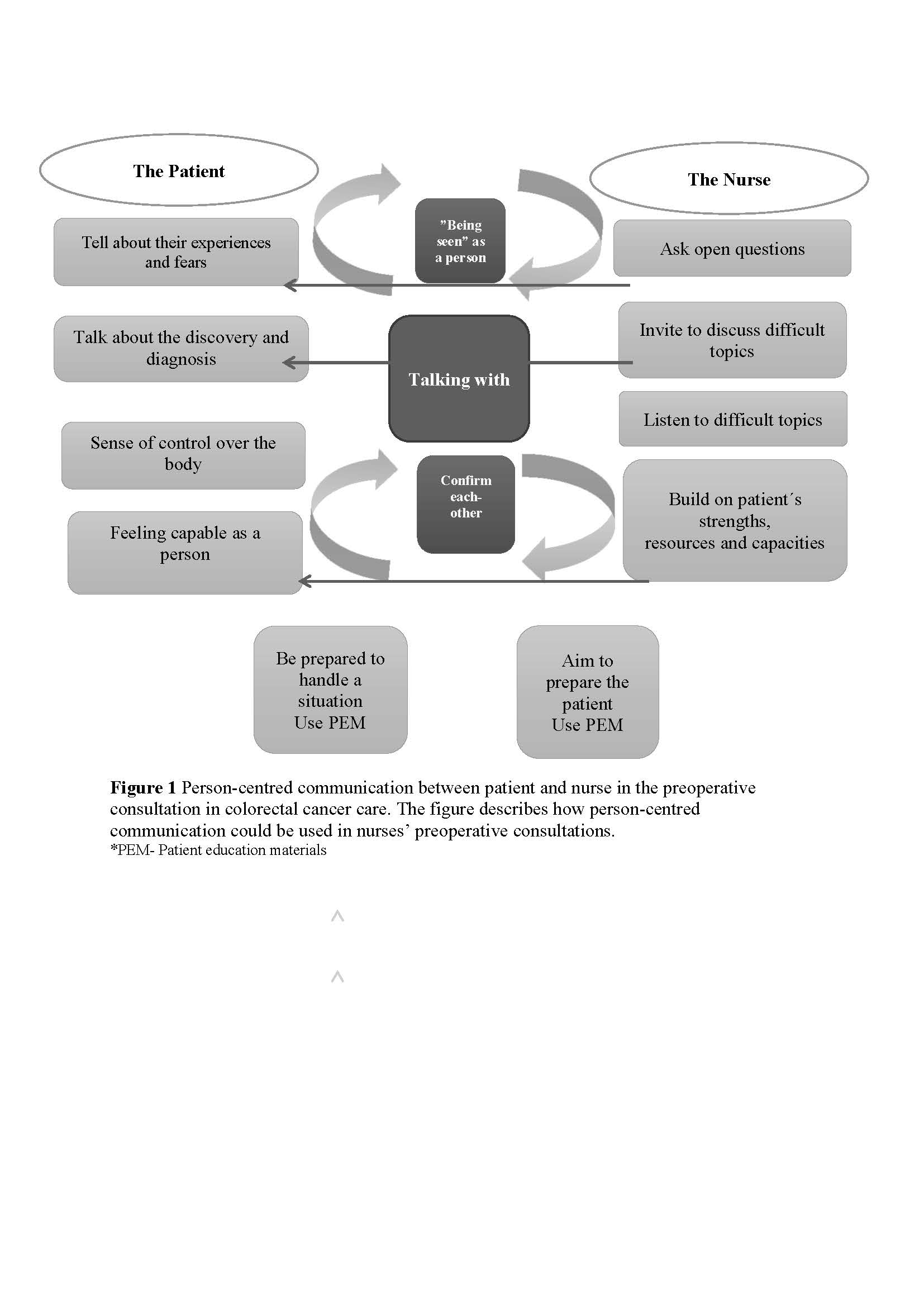
Did you notice any difference in those consultations where the PEM was used? We observed two types of dialogues: one type where the nurse was talking to the patient and another one where the nurse was talking with the patient. In a figure that we created, we describe how a person-centred communication can look (please see the image below). It shows that the health care professional should talk with the patient, confirm him/her, invite him/her into the consultation, and see him/her as a person. Both parties should confirm each other. The health care professional has to ask open-ended questions and build on the patient’s resources instead of just focusing on the problems. This will result in the patient feeling capable and getting him/her involved in a very different way.
The figure has been very useful in the specialist nurse training for which I am the Programme Co-ordinator here at the Institute of Health and Care Sciences at Sahlgrenska Academy. It helps the students in learning the difference between helping the patient feel prepared and preparing the patient.
Seeing the patient as a person is so important, it makes all the difference. Many health care professionals keep saying:” There’s just not enough time”, but when you are with the patient, then you must be present and see him/her for whom he/she is.
INTERVIEW IN SWEDISH BY: JEANETTE TENGGREN DURKAN